VA Disability Ratings
VA Disability Rating
for Deep Vein Thrombosis
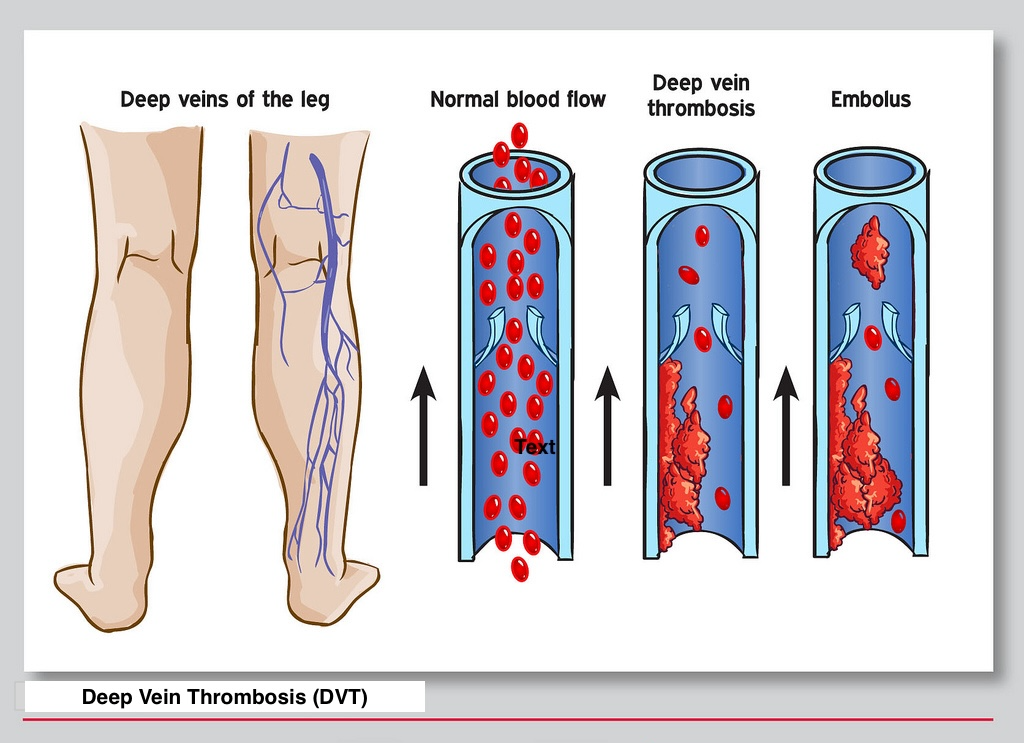
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, usually in the legs. DVT can lead to other serious complications, such as pulmonary embolism and edema. The VA provides benefits for service-connected DVT and blood clots with ratings between 0% and 100%. Read on to learn more about the DVT VA rating and what veterans who can’t work due to this health condition can do to receive additional compensation.
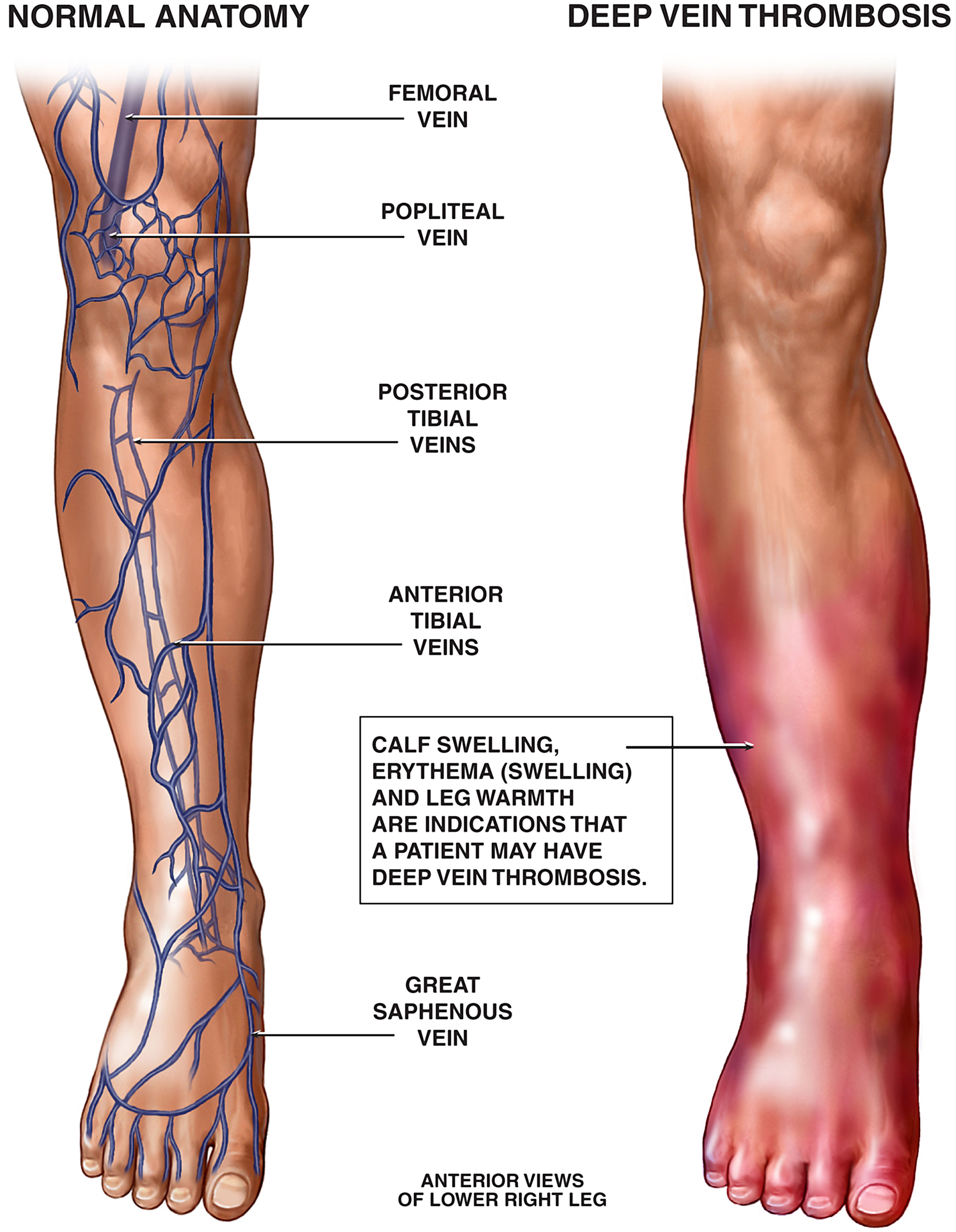
What is deep vein thrombosis?
Our bodies circulate blood through a complex system of arteries and veins. Hearts
pump blood into the body through the arteries, and veins bring blood back to the heart.
DVT VA rating
The VA rates DVT under diagnostic code 7121 in the Schedule of Ratings for “post-phlebitic syndrome of any etiology.” The VA rates most venous disorders under this code. A veteran’s rating under 7121 is based on the severity of their symptoms, including the level of swelling (edema), stasis pigmentation (discoloration), hardening (subcutaneous induration), and leaking or discharge (ulceration).
Description |
VA Rating |
Monthly Payment
|
|---|---|---|
Massive board-like edema with constant pain at rest |
100% |
$3,737.85 |
Persistent edema or subcutaneous induration, stasis pigmentation or eczema, and persistent ulceration |
60% |
$1,3161.88 |
Persistent edema and stasis pigmentation or eczema, with or without intermittent ulceration |
40% |
$1,3161.88 |
Persistent edema, incompletely relieved by elevation of extremity, with
|
20% |
$755.28 |
Intermittent edema of extremity or aching and fatigue in leg after prolonged
|
10% |
$171.23 |
Asymptomatic palpable or visible varicose veins |
0% |
None |
VABC for DVT
Symptoms of DVT can make it challenging to find and keep work. Veterans with DVT may struggle to sit and stand comfortably. They may also be more likely to experience mental health and sleep disorders that can make working even more difficult, if not impossible.
Veterans with DVT or other service-connected conditions that prevent them from maintaining “substantially gainful employment” may be entitled to (VABC) benefits.
VABC provides a pathway for veterans to receive the same compensation as a 100% rating, even when their symptoms do not meet the criteria for a schedular 100% rating.